A whole new set of rules that come with pregnancy: avoid the kitty litter box (to reduce the risk of toxoplasmosis) sleep on your side (to avoid compressing the vena cava), take your multivitamin every day, and a whole host of nutritional recommendations related to everything from unpasteurized dairy to moderating your fish intake. But how many of these “rules” are based in good science? How much evidence actually exists? Here, we review commonly cited rules and regulations of diet during pregnancy, and determine if they’re based in fact (true risk), fiction, or something in-between. First up: mercury exposure from shellfish and finfish.
Rule: Avoid fish high in mercury to avoid fetal cognitive defects
Mercury consumption is linked to interference in fetal brain and neurodevelopment, which, at certain levels, can lead to cognitive delays and neurological defects3. Most mercury exposure from our diets is in the form of methylmercury (MeHg), an environmental pollutant in aquatic ecosystems that contaminates our food supply through both natural and man-made (often manufacturing) sources3. In the environment, inorganic mercury is converted to MeHg primarily through bacterial activity. This MeHg can then accumulate in both finfish and shellfish to varying degrees via biomagnification8. Due to the increased impact of biomagnification moving up the food chain, MeHg levels are generally higher in apex predators such as Shark, swordfish, king mackerel, and tilefish – the precise species that are on the “avoid” list during pregnancy5.
Impacts of MeHg exposure
For most adults, the levels of MeHg in the normal food supply isn’t a concern. However, research has linked MeHg exposure to both brain and neurological defects in the developing fetus. This can be attributed to MeHg building up in the bloodstream over time, particularly in pregnant women and children. These sensitive groups are therefore at higher risk for adverse effects of high levels of circulating MeHg. This can cause symptoms ranging from mild to severe, such as paresthesia, ataxia, dysarthyria, hearing defects, visual disturbances, and even death3. Fetuses are considered the most sensitive subpopulation because of the vulnerability of their developing nervous system11. For fetuses in particular, prenatal poisoning with high dose MeHg is linked to intellectual disabilities and cerebral palsy12.
What does the science actually say about prenatal exposure to MeHg?
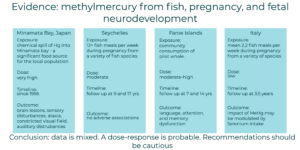
The detrimental effects of MeHg are typically considered dose-dependent – higher levels of exposure are linked to more severe effects2. In well-documented cases of congenital MeHg poisoning, significant and severe brain lesions were observed in fetuses whose mothers consumed high levels of MeHg during pregnancy. For example, a chemical plant spilled significant amounts of mercury into local Minamata Bay in 1956. Minamata bay represented a significant food source for residents of Minamata City, Japan10. In another high exposure incident in 1971-72, rural Iraqi children were poisoned via the consumption of bread made from mercury-treated grain seed2. These children experienced significant neurotoxicity in a dose-response fashion, with higher levels of exposure resulting in more significant impacts. Those who had the most severe levels of poisoning also experienced the least recovery in symptoms over the course of follow-up.
The dose-response nature of the relationship suggests that at lower levels of MeHg exposure, more subtle signs of cognitive or neurological defects could occur. This observation has been recognized by others, including the World Health Association Joint Expert Committee on Food Additives (2003) and the National Academy of Science’s National Research Council (2000). It also suggests that there may be concern that MeHg can cause more subtle developmental delays or neurological effects at low levels of exposure such as those consistent with the usual patterns of fish consumption seen in the US.
To investigate this, two large studies were performed in the Seychelles and Faroe Islands to investigate MeHg exposure in normal seafood consuming populations. In the Seychelles study, most MeHg exposure came from finfish consumption. The MeHg levels in these fish were similar to those from commercially available fish in the US12. Pregnant mothers consumed an average of 12 fish-based meals per week (a substantially larger amount of fish than averages in the United States). They were then followed through delivery and their children were evaluated 9 and 17 years of age13,6. The children showed no cognitive deficiencies at either follow-up point. The authors concluded that there is not enough evidence to support a neurodevelopmental risk from prenatal MeHg exposure resulting solely from ocean fish consumption.
However, a similar study in the Faroe Islands9 found that prenatal exposure to MeHg resulted in pronounced neurological dysfunction in language, attention, and memory at 7 years of age. They also observed dysfunction to a lesser extent in visuospatial and motor functions at the same age. These effects persisted in the long-term and were observed at a follow-up at 14 years old7. These authors concluded that even at “safe” levels, prenatal exposure to MeHg impacts development – even at levels currently considered safe. A notable difference between these studies is that the population in the Faroe Islands receive most of their dietary MeHg exposure through the consumption of pilot whale (Globicephala spp.) meat, while the population in Seychelles have a more diverse diet of various marine finfish. As such, the possibility remains that the source of the exposure (and in particular, the consumption of pilot whales) could differentially impact neurodevelopment.
Some research supports this hypothesis – including some recent work by Castriotta and colleagues. In this study, the consumption of MeHg in conjunction with selenium was evaluated4. This study showed high levels of antagonism between MeHg and selenium, and the authors concluded that selenium may counterbalance the negative effects of MeHg. Further, they suggest that the ratios of selenium to MeHg in various fish species should be considered when evaluating the risk of seafood consumption during pregnancy as these ratios can vary widely.
Recommendations for fish consumption during pregnancy
While the relationship between MeHg exposure and neurological developmental concerns is well established, the particular role that fish consumption plays in this remains unclear. These issues therefore remain as sticking points in the development of evidence-based recommendations regarding the consumption of fish and seafood during pregnancy. This is primarily due to the lack of clarity in just how neurotoxic prenatal exposure to MeHg is and how the source of MeHg modulates that impact.
As such, the Food and Drug Administration (FDA) and Environmental Protection Agency (EPA) have produced extensive literature on the MeHg concentrations in various fish species, and use that to produce highly conservative recommendations on just how much MeHg from fish is safe for pregnancy. They determined a reference dose that would be safe for an average pregnant woman and then included a 10-fold uncertainty factor to ensure that consumption levels will be well under the dose needed to cause neurodevelopmental effects. The calculation includes the EPAs estimated reference dose for chronic oral exposure to MeHg of 0.1 µg/kg body weigh/d, an average body weight of 75 kg (based on US NHANES data for pregnant women), and an average serving size of 4 oz of fish. You can review the specifics of the calculations used here.
From this:
- the highest allowable MeHg levels in fish per serving when eating 3 servings per week is 0.15 µg/g. (This calculation or “screening value” exists for 0-2 servings per week as well)
- Based on screening values and the average concentration of MeHg in a given fish species, any fish with an average mercury concentration less than or equal to 0.15 µg/g is rated as “Best Choices – eat 2 to 3 servings a week”.
- Similarly, any fish with an average mercury concentration greater than 0.46 µg/g was placed in the “Choices to Avoid” category (Administration, 2020). Based on this rating, the fish that the FDA recommends pregnant women avoid altogether are:
- King mackerel
- Marlin
- Orange roughy
- Shark
- Swordfish
- Tilefish from the Gulf of Mexico
- Bigeye tuna
Of the 63 fish species evaluated, the majority fall into the “Best Choice” category, where up to three (4 oz)servings per week are recommended. The FDA’s table can be found here if you would like to investigate this more fully. Fish remains an important source of omega-3 fatty acids, and most experts recommend eating seafood for this purpose, particularly during pregnancy5.
The takeaway:
Low-level MeHg exposures from maternal consumption of fish have not been consistently associated with adverse neurodevelopmental outcomes12. Additionally, the link between dietary MeHg and neurodevelopmental delays remains unclear. For this reason, a conservative recommendation that pregnant women avoid fish known to be high in MeHg has been developed.c
So, does science support this recommendation?
Evidence suggests support, but many factors remain unclear. In the absence of a full scope of evidence, this is one rule that women should probably adhere to during pregnancy out of caution.
Next Up: Sub, hoagie, torpedo, hero, or grinder – what’s the scoop on deli meats and listeriosis?
 About the author: Kimberly Lackey is a writer and consultant for Traverse Science®. If you want to learn more, follow her and Traverse Science on LinkedIn and connect with us at engage@traversescience.com.
About the author: Kimberly Lackey is a writer and consultant for Traverse Science®. If you want to learn more, follow her and Traverse Science on LinkedIn and connect with us at engage@traversescience.com.
About the company: Traverse Science® is a nutrition consulting firm working with ingredient suppliers and consumer packaged goods companies in the human and animal nutrition space. We work with clients to get science done, whether that means organizing and conducting a study, analyzing new or long-forgotten data, or writing a manuscript for peer review or guidance document for internal use. As teams change, time runs short, or projects pivot, we provide the muscle and the know-how to finish your nutrition science and get your projects out the door – whatever that means for you. We believe that science doesn’t have to be hard, and we’re here to make it easy.
References
- Administration F and D. Technical Information on Development of FDA/EPA Advice about Eating Fish for Women Who Are or Might Become Pregnant, Breastfeeding Mothers, and Young Children. 2020.
- Amin-zaki L, Majeed MA, Clarkson TW, Greenwood MR. Methylmercury poisoning in Iraqi children: clinical observations over two years. British Medical Journal. 1978;1(6113):613. doi:10.1136/bmj.1.6113.613
- Carrington CD, Montwill B, Bolger PM. An intervention analysis for the reduction of exposure to methylmercury from the consumption of seafood by women of child-bearing age. Regulatory Toxicology and Pharmacology. 2004;40(3):272–280. doi:10.1016/j.yrtph.2004.07.006
- Castriotta L, Rosolen V, Biggeri A, Ronfani L, Catelan D, Mariuz M, Bin M, Brumatti LV, Horvat M, Barbone F. The role of mercury, selenium and the Se-Hg antagonism on cognitive neurodevelopment: A 40-month follow-up of the Italian mother-child PHIME cohort. International Journal of Hygiene and Environmental Health. 2020;230:113604. doi:10.1016/j.ijheh.2020.113604
- Clinic M. Pregnancy and fish: What’s safe to eat? 2019. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy-and-fish/art-20044185#:~:text=While%20pregnant%20women%20can%20get,been%20shown%20to%20cause%20problems.
- Davidson PW, Cory-Slechta DA, Thurston SW, Huang L-S, Shamlaye CF, Gunzler D, Watson G, Wijngaarden E van, Zareba G, Klein JD, et al. Fish consumption and prenatal methylmercury exposure: Cognitive and behavioral outcomes in the main cohort at 17 years from the Seychelles child development study. NeuroToxicology. 2011;32(6):711–717. doi:10.1016/j.neuro.2011.08.003
- Debes F, Budtz-Jørgensen E, Weihe P, White RF, Grandjean P. Impact of prenatal methylmercury exposure on neurobehavioral function at age 14 years. Neurotoxicology and Teratology. 2006;28(5):536–547. doi:10.1016/j.ntt.2006.02.005
- Drouillard KG. Encyclopedia of Ecology. Ecotoxicology: Article Titles: B. 2008;(Environmental Science and Technology412007):441–448. doi:10.1016/b978-008045405-4.00377-3
- Grandjean P, Weihe P, White RF, Debes F, Araki S, Yokoyama K, Murata K, SØRENSEN N, Dahl R, JØRGENSEN PJ. Cognitive Deficit in 7-Year-Old Children with Prenatal Exposure to Methylmercury. Neurotoxicology and Teratology. 1997;19(6):417–428. doi:10.1016/s0892-0362(97)00097-4
- Harada M. Minamata Disease: Methylmercury Poisoning in Japan Caused by Environmental Pollution. Critical Reviews in Toxicology. 2008;25(1):1–24. doi:10.3109/10408449509089885
- Mahaffey KR. Recent advances in recognition of low-level methylmercury poisoning. Current Opinion in Neurology. 2000;13(6):699–707. doi:10.1097/00019052-200012000-00015
- Myers GJ, Davidson PW. Prenatal methylmercury exposure and children: neurologic, developmental, and behavioral research. Environmental Health Perspectives. 1998;106(suppl 3):841–847. doi:10.1289/ehp.98106841
- Myers GJ, Davidson PW, Cox C, Shamlaye CF, Palumbo D, Cernichiari E, Sloane-Reeves J, Wilding GE, Kost J, Huang L-S, et al. Prenatal methylmercury exposure from ocean fish consumption in the Seychelles child development study. The Lancet. 2003;361(9370):1686–1692. doi:10.1016/s0140-6736(03)13371-5
- Joint Expert Committee on Food Additives (JECFA) of the Food Agriculture Organization and the World Health Organization (2003). http://www.who.int/pcs/jecfa/Summary61.pdf.
- National Research Council (NRC) of the National Academy of Sciences (2000). Toxicological Effects of Methylmercury, National Academy Press, Washington, D.C.